
| JUNE 15, 2024 (Saturday) *Date/Time in Japan Standard Time | ||
| 16:30-17:00 | Registration | Building A B1F B103 |
|---|---|---|
| 17:00-18:00 | ASAIHL Board meeting (Board members only) | Building A B1F B103 |
| 18:30-20:30 | Dinner (Board members Only) | |
| Day 1: JUNE 16, 2024 (Sunday) | |
| 9:00-9:30 | Registration |
|---|---|
| 9:30-10:00 | Opening remarks |
| 10:00-12:00 | |
| 12:00-13:00 | |
| 13:00-18:00 | Country report, presentation, |
| 18:30-20:30 | |
| Day 2: JUNE 17, 2024 (Monday) | |
| 9:00-12:00 | country report |
|---|---|
| 12:00-13:00 | |
| 13:00-16:45 | Country report, presentation, DYNAMEID meeting |
| 17:00-17:30 | Closing ceremony |
| Day 3: JUNE 18, 2024 (Tuesday) | |
| 8:30-18:00 | Optional tour ※Closed due to enrollment reached to the limit. |
|---|---|

Reforms in the way physicians work are now having a major impact on medical education and research. University hospital physicians, who play a central role in medical education and research in Japan, originally worked long hours. Since the national universities became independent in 2004, the amount of time spent on medical treatment has increased significantly, and the amount of time spent on research has been decreasing rapidly. Japan's medical research capacity has declined significantly, and it is an extremely important issue to ensure that university faculty members, whose time is taken up by clinical work, have more time for education and research. For this reason, the Ministry of Education, Culture, Sports, Science and Technology (MEXT) and the Ministry of Health, Labor and Welfare (MHLW) are collaborating to implement government-wide policies to support university hospitals.This presentation will introduce the progress of current discussions on the future of medical education and research in Japan.

In recent years, the integration of Artificial Intelligence (AI) in healthcare has revolutionized diagnostic processes, enhancing the speed and accuracy of medical assessments. Particularly, the advent of conversational AI has opened new avenues for patient interaction and data collection. However, this rapid advancement brings forth significant challenges, primarily concerning the accuracy and reliability of generated content, ethical considerations, and the safeguarding of patient data. In this lecture, we will explore the evolution of AI technologies in the medical field, emphasizing the challenges faced by current conversational AI systems. We will delve into specific issues within healthcare applications of AI technologies by customizing Large Language Models. Further, I will introduce our ongoing research efforts focused on developing patient-centered diagnostic reasoning systems that respect and incorporate patient narratives, highlighting preliminary findings and case studies. The importance of collaboration between engineering and medical fields will be stressed, arguing that such partnerships are crucial for advancing AI technologies that are both innovative and ethically responsible. Our discussion aims to foster a deeper understanding of the potential and limitations of AI in healthcare, encouraging continued education of health care professionals and innovation that places patient perspectives at the forefront.
Diagnostic Excellence (DEx) refers to achieving optimal patient care through accurate and rapid diagnosis, maximizing patients' experience. The emphasis on DEx arises because the quality of diagnosis holds a critically important position in the overall quality and safety of healthcare. This concept has been featured in major global medical journals such as JAMA and BMJ in recent years. What are the elements necessary for educating physicians in realizing DEx? This presentation will explore educational methods to enhance the diagnostic abilities of individual physicians, which are central to DEx. Such an analytical approach to education will, I believe, result in a message that is not only relevant to physicians but also domain-general, as the formalization techniques discussed can be applied across various fields from education perspective. The presentation will also address the collaboration and challenges between technology and diagnosis education, which are themes of this conference.

Society 5.0, proposed by the Japan's National Institute of Advanced Industrial Science and Technology, entails a human-centered society with an integrated cyber- and physical space aimed to resolve social challenges and promote economic growth. Medical care in Society 5.0 is highly individualized to enable lifelong, anticipatory healthcare for each patient and citizen with minimal intrusion. Developments in big data and artificial intelligence (AI) allowed high accuracy, high speed analyses at rates previously unheard of. Hence, the medical field is anticipating deeper understanding of pathologies, as well as realization of ubiquitous and human-centered medicine through values embedded in P4 (predictive, personalized, preventive, and participatory) medicine. Mobile health (mHealth) refers to the “use of mobile and wireless technologies to support the achievement of health objectives.” Among mHealth categories, smartphone applications (apps) appear well-suited in collecting electronic patient-reported outcomes (ePROs), which gained attention as a novel, unintrusive route to evaluate symptoms of chronic illnesses. In this lecture, I aim to provide a synopsis of healthcare in Society 5.0 with discussion on the future of data science in medicine by illustrating ongoing efforts on dry eye disease and hay fever using smartphone app-based stratification strategies for subjective symptoms and disease phenotypes.

In 2022, the World Health Organization (WHO) reported that the full death toll associated with the COVID-19 pandemic was approximately 15 million, while before the COVID-19 pandemic 13.7 million infection-related deaths were reported in 2019, mainly in low-income countries. Infectious diseases are significant burdens on public health and the economic stability of developing countries. These diseases are the leading cause of death and disability and present growing challenges to health security and human progress. Education is considered a key social determinant of health because it can aid in the fight against global infections. It has been demonstrated that enhancing health education regarding infectious diseases is crucial in promoting comprehensive prevention and control measures. Nevertheless, children across many underdeveloped and developing countries have limited access to quality education. Sub-Saharan Africa has the highest rates of education exclusion worldwide because over one-fifth of primary-age children are out of school, and almost 60 percent of youth between the ages of 15 and 17 are not in school. In this lecture, the speaker, born from Africa, will describe his fight for access to quality education to finally become a health professional. Education is the most powerful weapon we can use to change the world.

Medical tourism, in its most fundamental definition, involves provision of medical care to non-native patients who may have different health care needs and expectations to the host population. Successful medical tourism endeavours have sought to understand these unique needs, in order to meet health care expectations of inbound patients seeking care. As Japan seeks to enter the medical tourism market, this may be particularly challenging, given both the relatively homogenous nature of Japanese society and its strictly standardized health system. In this cross-sectional study using social media, we analyzed self-reported data from 553 foreign patients living in Japan (mean age, 33.6 years; 70.5% women) to investigate patterns and perceptions of medical care in Japan by non-Japanese patients living in Japan, with a focus on assessing reasons for delay of care. The majority of patients received care from community clinics, with only a small number of foreign patients receiving care from a hospital-based outpatient clinic. Apart from those reporting only a single healthcare encounter in the last 12 months, the majority of whom received care from a hospital outpatient clinic, the majority of foreign patients experiencing multiple healthcare visits reported receiving these at community clinics. Approximately 70% of respondents reported being satisfied with healthcare services in Japan, a slightly higher percentage than those reporting satisfaction with care in their home country. Nonetheless, 53% of respondents reported delaying care in Japan versus only 33.5% in their home country. Language barriers were reported most commonly as a reason for delay (17.4%), followed by perception of care inadequacy (11.3%). Delayers were significantly more likely to be women (75.4% vs 64.8%, p=0.007). Delay was less likely if friends (rather than co-workers or family) were reported as the primary health care support (36.5% vs 28.7%; p=0.008), suggesting the need for local support in order to access care. Self-reported health care concerns included lack of mental healthcare, lack of care regarding lifestyle diseases, and healthcare costs. An understanding of local needs and barriers to care may help inform design and implementation of successful medical tourism systems in the future. Our small study suggests that health systems in Japan for non-Japanese patients, including medical tourists, may be more successful by improving language competency by providers, as well as focusing on personalized support to promote access and decrease mental duress.

The Japanese government considers medical inbound business as one of the international developments in Japan's healthcare sector. The promotion of medical inbound tourism is increasing annually, and there is an expectation of significant growth in medical tourism globally. Fujita Health University currently offers medical tourism services at two locations: the Fujita Medical Innovation Center Tokyo, which specializes in health checkups and advanced medical care, and the Fujita Health University International Medical Center, which caters to patients seeking advanced treatments such as surgery, chemotherapy, and rehabilitation in Japan. In 2019, approximately 600 individuals were examined at our center. However, the number of patients visiting Japan drastically declined due to travel restrictions imposed during the COVID-19 pandemic. Since 2020, online second opinions have been conducted, resulting in 120 online consultations in 2020 and 140 in 2021. In 2023, when travel restrictions were completely lifted, the number of consultations increased to 360, with most patients traveling to Japan for medical treatment. Our hospital holds several certifications for treating not only inbound patients but also foreign patients, providing regular medical care for foreign patients residing in Japan. At our center, in addition to a dedicated entrance for inbound patients, nurses and staff, four medical interpreters, including graduates from the Fujita Health University Graduate School Medical Interpretation Course, are stationed to assist patients speaking different languages. Drawing from our experience, we will continue to evaluate the trajectory of medical tourism in Japan.


In 2020, there was a global outbreak of the new coronavirus infection (COVID-19), and although there were initially no effective drugs, various vaccines, including mRNA vaccines, were made progress. mRNA vaccine technology is currently being applied to various vaccines, and vaccine development is progressing for several infectious diseases. This seminar will introduce the development and clinical application of new vaccines.

Healthcare workers are potentially exposed to various infectious diseases, necessitating proper health management. We will discuss the importance of vaccinating staff, specific implementation methods, and strategies to improve vaccination rates. We will focus on the role of vaccination in preventing infections and ensuring workplace safety, and introduce its promotion as part of health management.
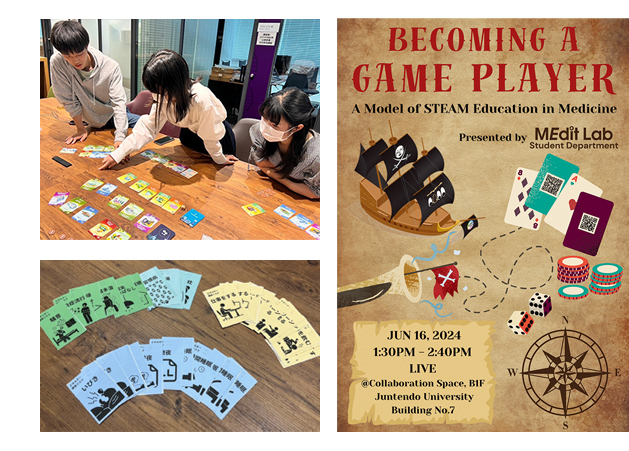
In these challenging and unpredictable times, we need liberal arts, which involves integrating and considering all information about questions without definitive answers. MEdit Lab (Juntendo University STEAM Education Research Association) operates under the concept of "Medicine as Liberal Arts". The members of the MEdit Lab Student Department participate in game-making workshops organized by MEdit Lab and hold regular meetings to focus on student-led game creation. Through the process of making games related to medicine—researching themes, learning mechanisms, and engaging in trial and error—they learn how to learn and understand liberal arts in a practical form. In this session, MEdit Lab Student Department members will present their learning and achievements through game-making. They will also interact with participants while playing the medical learning game they created as an achievement and demonstrate a way of learning through games. The activities of the MEdit Lab Student Department epitomize STEAM education by combining the knowledge they have gained to create new things and contribute to society. We hope that our activities will serve as a role model for innovative medical education.
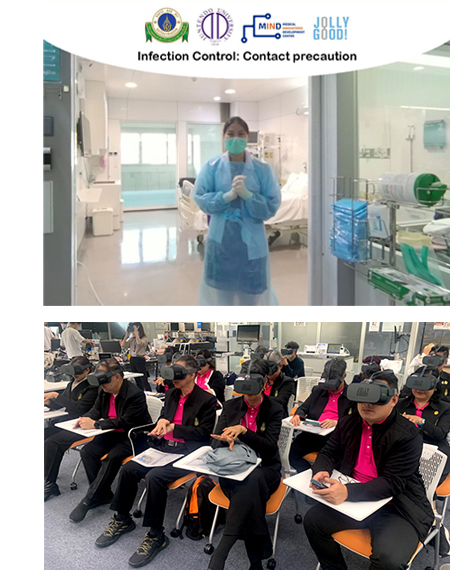
Virtual reality (VR) is currently being used in medical education. Juntendo University started VR to provide infectious disease education during the COVID-19 outbreak. Originally, VR is suitable for surgical and emergency training. It is now clear that VR can be used for education in a variety of professions, including internal medicine, rehabilitation, and geriatric medicine. Currently, Juntendo University is collaborating with Mahidol University, Thailand on an international joint research and education project related to medical education. In this workshop, participants will experience medical education using VR. We will discuss its potential as an educational tool for geriatric care multidisciplinary training, which is an issue in Japan and around the world.

VENUE : Hotel Tokyo Garden Palace 2nd floor "Takachiho hall"